One Thing

One Thing
Stormin’
- https://www.youtube.com/watch?v=9WEJT6ZMvIY
- https://www.youtube.com/watch?v=JWkoioJ7QDo
- https://www.youtube.com/watch?v=psbxQMG6HLY
- https://www.youtube.com/watch?v=piCAXfEFBwk
- https://www.youtube.com/watch?v=eMfw81LWokI
- https://www.youtube.com/watch?v=cSCTqSfi1Vg
- https://www.youtube.com/watch?v=VDOhbrU29ZM
=====
The Big Picture (So We Don’t Miss the Point)
Your objectives
- Transition to a carnivore-leaning diet without shock
- Lower blood glucose consistently
- Reduce insulin resistance
- Create conditions where medications may become unnecessary (under supervision)
Key principle
Food changes fast. Medications must change slowly.
That’s how people succeed without crashes, hypoglycemia, or rebound binges.
Phase 1: Stabilize First (Weeks 1–2)
Goal: Stop blood sugar spikes and cravings before going full carnivore.
What you eat
- Meat at every meal
- Eggs, butter, animal fats
- Low-carb vegetables only if needed (leafy greens, zucchini, cucumbers)
- Zero sugar
- Zero grains
- Zero seed oils


What you remove immediately
- Bread, rice, pasta, cereal
- Fruit and juice
- Sweets (even “healthy” ones)
- Soda and sweetened drinks
What this does
- Blood sugar becomes predictable
- Hunger calms down
- You stop riding the glucose roller coaster
📌 Daily rule:
If it didn’t come from an animal, question it.
Phase 2: Keto → Carnivore Bridge (Weeks 3–6)
Goal: Train your metabolism to run on fat instead of glucose.
What changes
- Vegetables taper down
- Meals simplify
- Protein + fat become dominant
Typical day
- Breakfast: eggs + butter
- Lunch: ground beef or sardines
- Dinner: steak, pork, lamb, or chicken thighs
- Salt generously
- Drink water (add electrolytes)


Blood sugar expectation
- Fasting glucose begins trending down
- Post-meal spikes flatten
- Energy becomes steadier
⚠️ Important
If you’re on insulin or sulfonylureas, this is where medication adjustments often become necessary. Many people experience lower glucose than expected.
This is not failure.
This is success that needs supervision.
Phase 3: Full Carnivore Reset (Weeks 7–12)
Goal: Remove remaining triggers and inflammation.
What you eat
- Beef, lamb, pork, poultry, fish
- Eggs (if tolerated)
- Butter, tallow, ghee
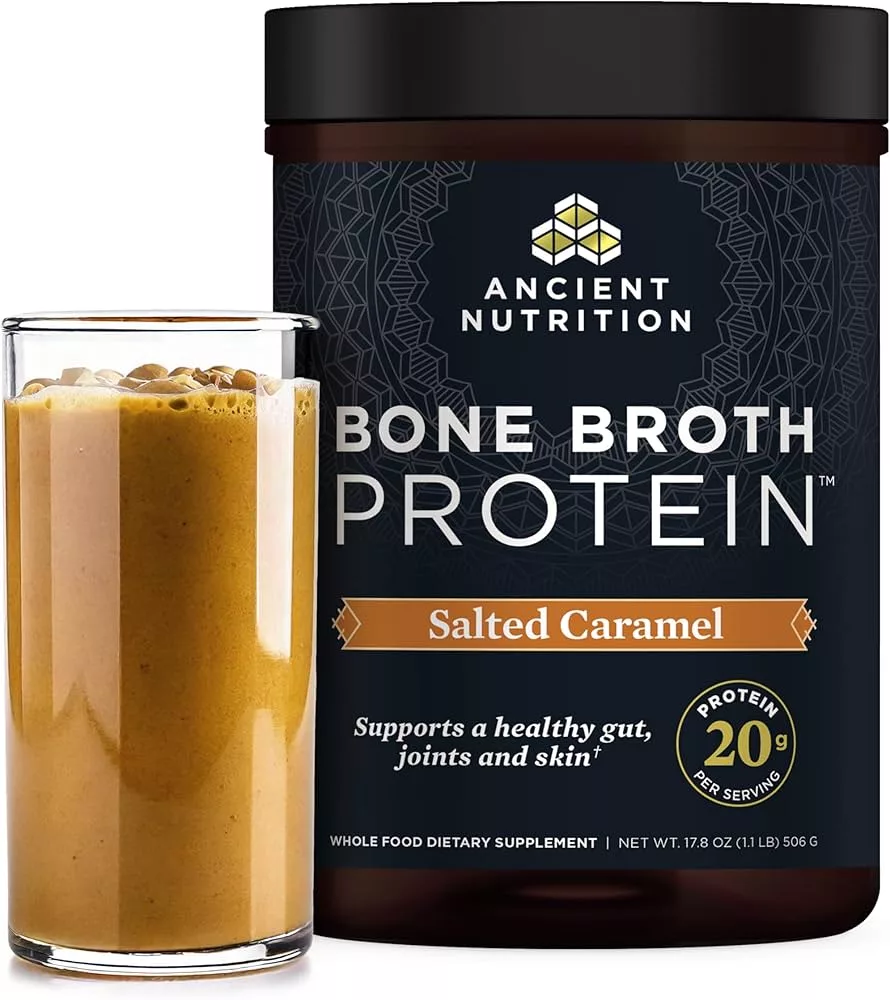
- Bone broth
- Salt
What’s gone
- Vegetables
- Sweeteners (even keto ones)
- Nuts
- Dairy (except butter/ghee if needed)


What typically improves here
- Fasting glucose
- A1C (over time)
- Triglycerides
- Inflammation
- Hunger regulation
Medication Reduction Strategy (Non-Negotiable Safety Rule)
You do not “push through” meds.
Instead:
- Track fasting glucose daily
- Track post-meal glucose occasionally
- Bring data, not opinions, to your clinician
- Reduce meds only when numbers support it
Many people reduce:
- Insulin first
- Then sulfonylureas
- Metformin often last (or stays)
Non-Food Levers That Multiply Results
1. Walking (after meals)
- 10–20 minutes
- Blunts glucose spikes
- Improves insulin sensitivity
2. Sleep
- Poor sleep = higher glucose
- Treat sleep like medicine
3. Stress containment
- Chronic stress raises blood sugar
- Simple breathing beats supplements
What Success Actually Looks Like
Not:
- White-knuckling
- Obsessing over ketones
- Chasing perfection
But:
- Fewer cravings
- Calm energy
- Predictable glucose
- Less medication over time
- Confidence in your body again
Next Step (Your Choice)
PART 1: The Doctor Conversation Script
(Use this tone: calm, measured, collaborative)
Opening (sets the frame)
“I want to talk with you about improving my diabetes control in a way that’s safe given my stroke history. My goal isn’t to stop medications suddenly—it’s to reduce insulin resistance and see, over time, whether medication reduction becomes appropriate.”
This does three things:
- Signals safety
- Signals patience
- Signals respect for medical authority
State the Problem Clearly (without blame)
“Despite medications, my blood sugar has been difficult to keep consistently in range. I’d like to address the underlying insulin resistance, not just manage numbers.”
Doctors respond well to:
- “consistently”
- “underlying”
- “risk reduction”
Introduce Diet Without Trigger Words
Avoid saying “carnivore” at first.
“I’m planning to follow a very low-carbohydrate, animal-based elimination diet for a defined period, with careful glucose monitoring.”
If they ask why:
“Because carbohydrate restriction has the most immediate and predictable effect on glucose variability.”
That’s a clinical statement, not a belief.
Stroke-Specific Safety Framing (critical)
“Because of my prior stroke, balance, blood pressure stability, and avoiding hypoglycemia are my top concerns. I’m specifically asking for your help to make this safer, not riskier.”
This reframes the entire discussion.
The Ask (this is the key line)
“What I’d like is your guidance on:
- What glucose thresholds should trigger medication adjustment
- Which medications we would reduce first if numbers improve
- How often you’d want labs or check-ins during the transition”
Doctors like structured asks.
If They Push Back on the Diet
Don’t debate. Redirect.
“I understand this isn’t a standard recommendation. I’m not asking for endorsement—only supervision and risk management while I collect objective data.”
This is hard to argue against ethically.
Close with Partnership
“I want us to be working from the same data so I don’t accidentally over-medicate as my glucose improves.”
That sentence alone has saved many people from hypoglycemia.
PART 2: Stroke-Adapted Guardrails You Should Explicitly Mention
These show maturity and reduce resistance.
1. Hypoglycemia Prevention Plan
Say:
“Because of stroke risk, I will not tolerate low blood sugar events. I’ll be checking fasting glucose daily and post-meal readings initially.”
If on insulin or sulfonylureas:
“I’m aware reductions may be necessary sooner rather than later.”
2. Blood Pressure Stability
Very low carb diets can lower BP quickly.
Mention:
“I’ll be watching for lightheadedness or balance changes and will report them immediately.”
That reassures them you’re not ignoring red flags.
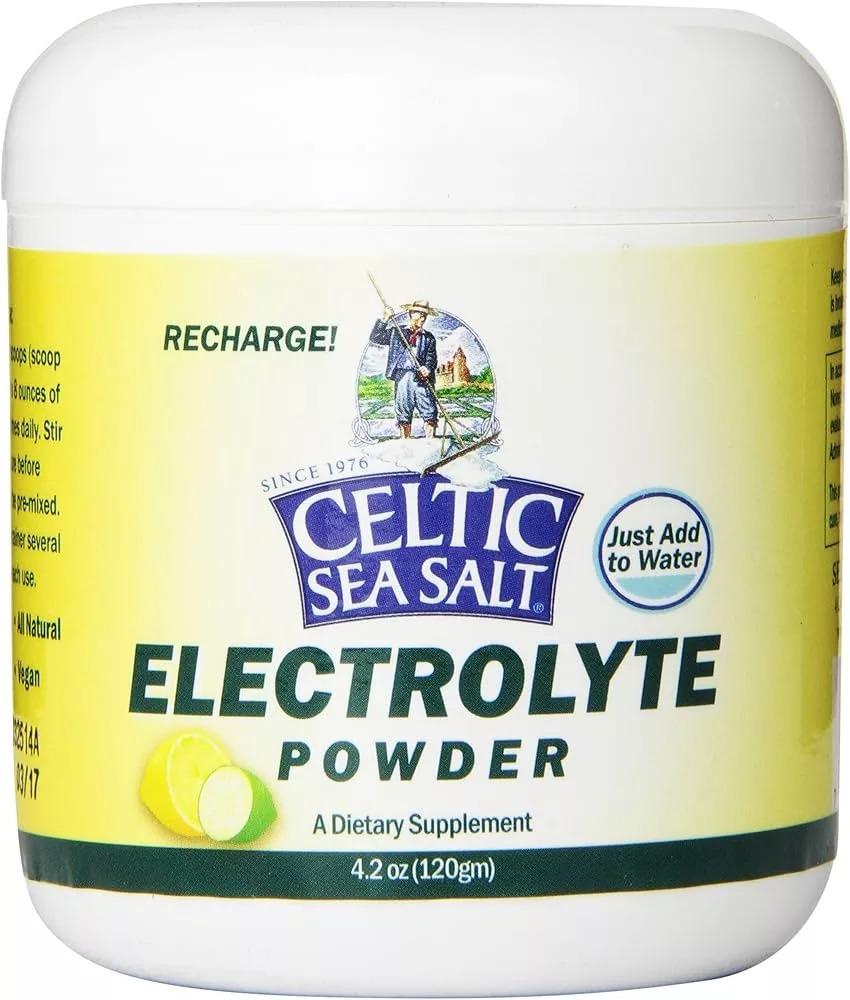
3. Electrolyte Awareness (huge for stroke + balance)
Say:
“I’ll be deliberately managing sodium and hydration to reduce dizziness or falls.”
Doctors love hearing this.
PART 3: Balance & Strength Adaptation (What You’re Doing Alongside Diet)
This matters more than the diet, in their eyes.
What to Say
“Alongside diet changes, I’m prioritizing:
– Daily walking for glucose control
– Light strength work for fall prevention
– Balance exercises to reduce stroke-related instability”
If you want a simple line:
“My goal is stability and function, not weight loss.”
That lands very well.
Safe, Doctor-Approved Movement Plan (you can mention this)
- Walking after meals (10–20 min)
- Sit-to-stand reps
- Wall-supported balance work
- No HIIT, no exhaustion
This frames you as risk-aware, not extreme.
PART 4: What NOT to Say (Very Important)
Avoid:
- “I read online…”
- “This cures diabetes”
- “I want to get off all meds fast”
- “Doctors don’t understand nutrition”
Those trigger shutdown immediately.
PART 5: If the Doctor Still Resists
Use this fallback:
“If you’re not comfortable supervising this, could you refer me to a clinician or dietitian experienced with low-carbohydrate diabetes management?”
That keeps momentum without confrontation.
PART 6: Your Quiet Advantage
You have:
- Age
- A stroke history
- A legitimate medical reason to avoid glucose swings
- A plan centered on monitoring, not ideology
That puts you in a strong negotiating position.
Excellent—this will be calm, conservative, and stroke-aware, not macho carnivore. The aim is stable blood sugar, steady blood pressure, and improved balance, with zero heroics.
Think of this as “Carnivore for neurological recovery and metabolic repair.”
Stroke-Safe Carnivore Starter Plan
(First 14 days — adjustable)
Design Rules (Why this works)
- No fasting (hypoglycemia risk)
- Regular meals (neurological stability)
- Deliberate electrolytes (fall prevention)
- Gentle movement (retrain balance, not exhaust it)
PART 1: Meals (Simple, Predictable, Repeatable)
Core Foods (Your entire menu)
- Beef (ground beef, chuck roast, ribeye)
- Eggs
- Butter or ghee
- Sardines or salmon (2–3x/week)
- Bone broth
- Salt

Daily Meal Structure (No guessing)
Breakfast (within 90 minutes of waking)
Option A
- 3 eggs cooked in butter
- Salt generously
Option B
- Leftover ground beef + butter
Why
- Prevents morning glucose dips
- Stabilizes cortisol
- Supports brain glucose needs post-stroke
Lunch
- 6–8 oz ground beef or steak
- 1–2 tbsp butter or tallow
- Salt
Optional (first 2 weeks only):
- A few bites of cucumber or spinach if digestion feels off
(This usually fades quickly.)
Dinner (earlier is better)
- 6–8 oz meat (rotate beef, pork, chicken thighs)
- Butter or fat
- Bone broth if appetite is low
If Blood Sugar Runs Low
- Add more fat, not carbs
- Eat sooner, not less
- Never “push through”
PART 2: Electrolytes (This Is Non-Negotiable)
Electrolytes are fall prevention, not supplements.
Daily Targets (safe starting point)
- Sodium: 4–6 grams/day
- Potassium: from meat + broth
- Magnesium: 200–400 mg (glycinate preferred, evening)
Simple Electrolyte Plan
Morning
- 1 cup water + ½ tsp salt
Midday
- Bone broth (salted)
Evening
- Magnesium supplement (if approved by your clinician)
⚠️ If dizziness or unsteadiness appears:
- Add salt first
- Sit before standing
- Report if persistent

PART 3: Stroke-Safe Balance & Strength Work
(10–15 minutes, 1–2x daily)
This is neural retraining, not exercise.
Daily Walking (After Meals)
- 10–20 minutes
- Flat ground
- Comfortable pace
- Focus on heel-to-toe
Why:
- Lowers post-meal glucose
- Improves gait confidence
- Enhances brain insulin signaling
Balance Circuit (Do Near a Wall or Counter)
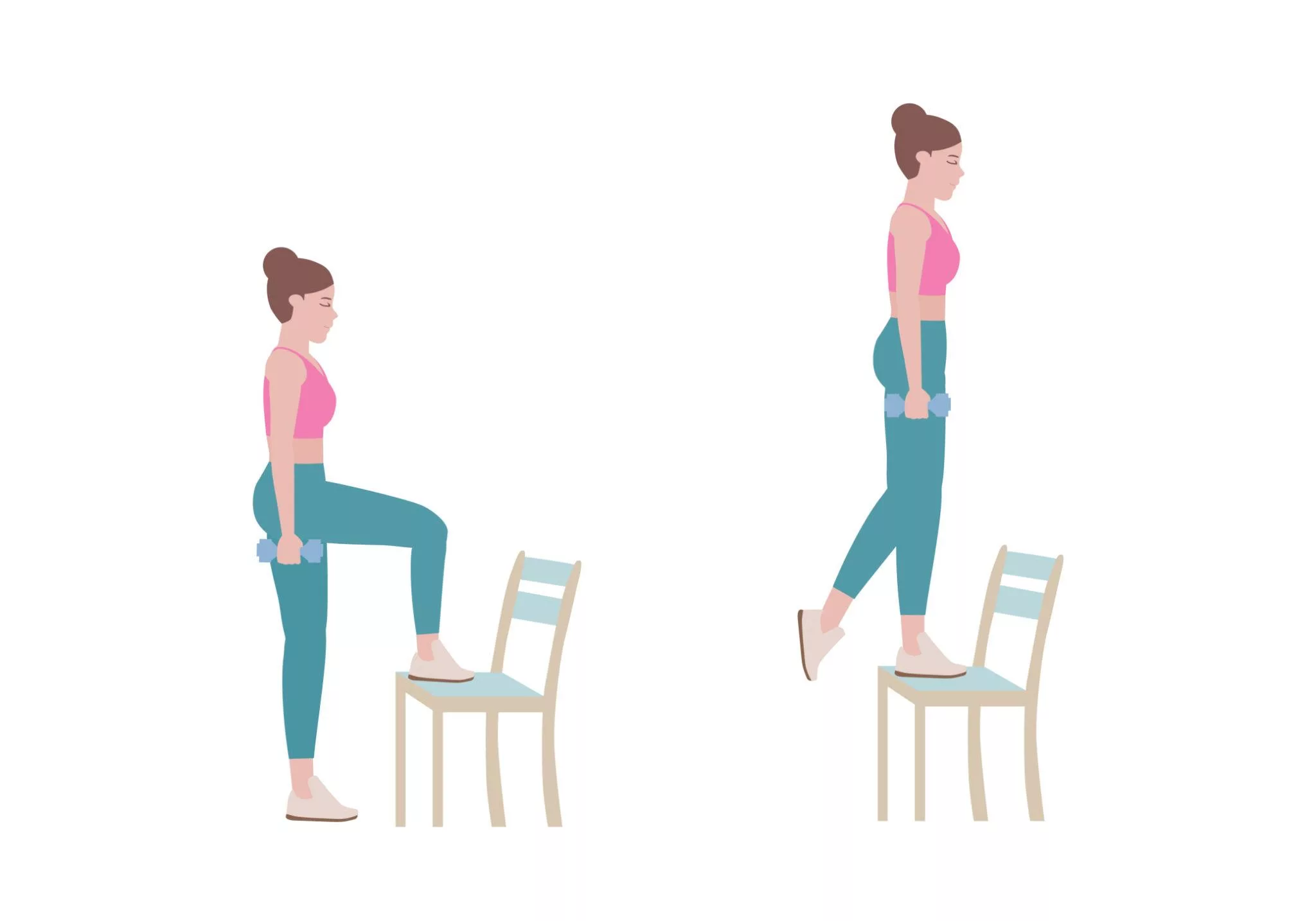


1. Sit-to-Stand (Foundation)
- 5–10 reps
- Use arms if needed
- Smooth, controlled
2. Supported Single-Leg Stand
- Hold counter
- 10–20 seconds each leg
- Eyes open only
3. Heel-to-Toe Walk
- 5–10 slow steps
- Turn and repeat
- Stop if dizziness appears
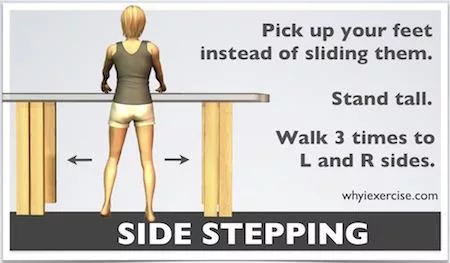
4. Standing Weight Shifts
- Shift weight side-to-side
- 10 reps
- Slow and deliberate
Frequency
- Once daily minimum
- Twice daily if energy is good
- Skip only if ill or unstable
PART 4: Blood Sugar & Safety Guardrails
Check
- Fasting glucose daily
- Post-meal glucose occasionally
Red Flags (Pause & Adjust)
- Lightheadedness on standing
- Shakiness or confusion
- Sudden weakness
- Vision changes
- Repeated glucose <70 mg/dL
If any occur:
- Eat
- Hydrate
- Salt
- Sit
- Notify clinician if persistent
PART 5: What “Success” Looks Like (First 2 Weeks)
- Fewer cravings
- Steadier energy
- Less urgency to snack
- Improved walking confidence
- More predictable glucose numbers
Not:
- Rapid weight loss
- Ketone chasing
- Medication changes without supervision
Optional (But Powerful)
- Eat the same meals for 7 days
→ removes variables - Keep a simple log:
- Meals
- Glucose
- Balance confidence (1–5)
Doctors respect logs.