Proprioceptive Decline
Proprioceptive Decline
That issue is surprisingly common in older adults, and it usually isn’t just “clumsiness.”
It’s most often tied to changes in visual-spatial perception—how the brain judges distance, depth, and height.
Here are the main conditions that cause it, from most common to more serious:
🧠 Depth perception impairment
Most common explanation
This happens when the eyes and brain no longer coordinate distance accurately.
Typical signs
- Misjudging curb height or stair depth
- Reaching too short or too far
- Trouble parking or stepping off sidewalks
- Feeling unsure on stairs or uneven ground
Common causes
- Cataracts
- Macular degeneration
- Diabetic eye disease
- Reduced contrast sensitivity with age

👀 Visual-spatial impairment
This is a brain processing issue, not just eyesight.
What’s happening
- Eyes may be “fine,” but the brain misinterprets space
- Often worsens in low light or cluttered environments
Seen with
- Normal aging (mild forms)
- Early cognitive changes
- Post-stroke changes
🧠 Proprioceptive decline
This is your internal body position sense fading a bit.
Results
- Legs feel “shorter” or steps feel “off”
- You think your foot cleared the step—but it didn’t
Often worsened by
- Neuropathy (especially diabetic)
- Muscle weakness
- Reduced ankle flexibility
Proprioceptive decline is a quiet but important part of aging—and it’s especially relevant if you’ve had a stroke, live with diabetes, or notice more clumsiness than you used to.
Let’s break it down in plain language and then get practical.
What Is Proprioceptive Decline?
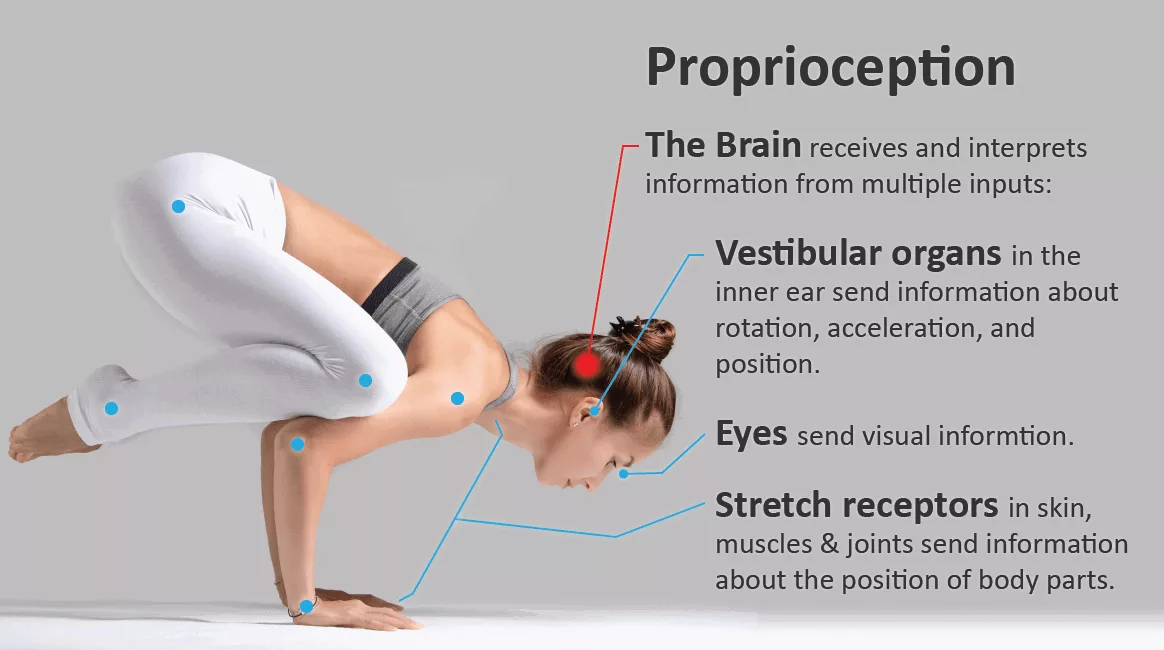
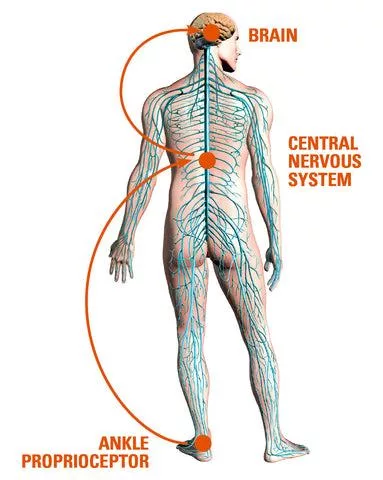
Proprioception is your body’s internal GPS.
It’s the sense that tells you:
- Where your feet are without looking
- How hard you’re gripping something
- Whether you’re upright, leaning, or about to lose balance
Proprioceptive decline happens when that internal feedback weakens.
Common signs:
- Tripping or misjudging steps
- Feeling unsteady in the dark or on uneven ground
- Dropping objects or over-gripping
- Slower reaction when you start to fall
- Needing to look at your feet to walk confidently
Why Proprioception Declines (Especially After 60)
![]()


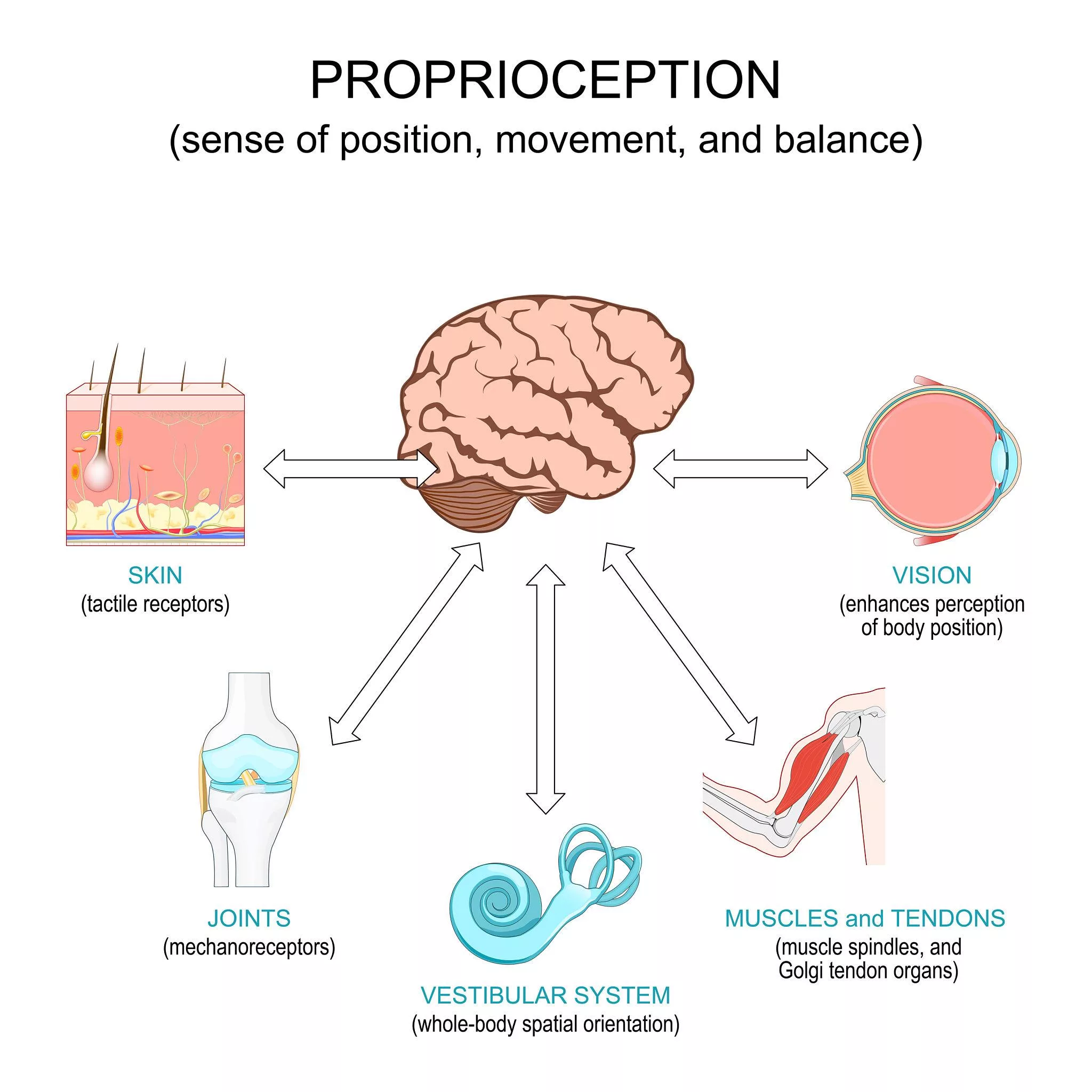
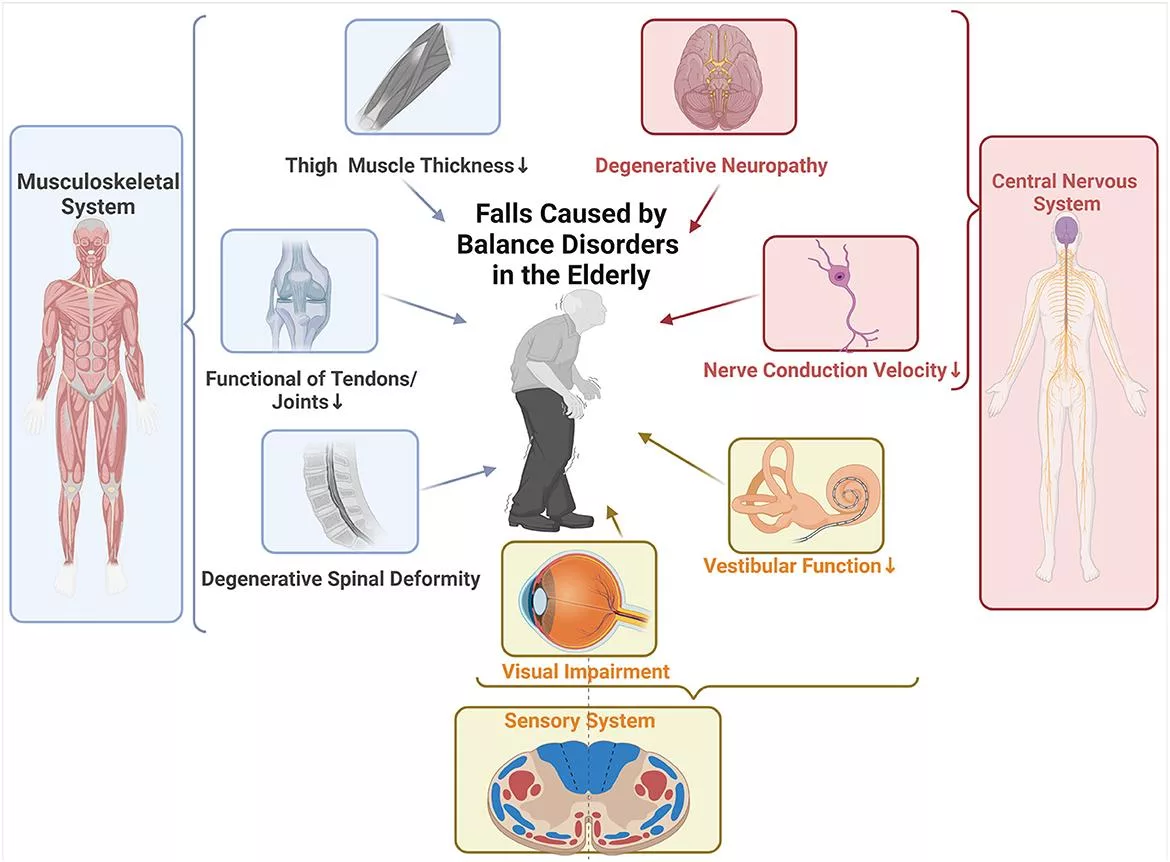
Several systems contribute—and they all age together:
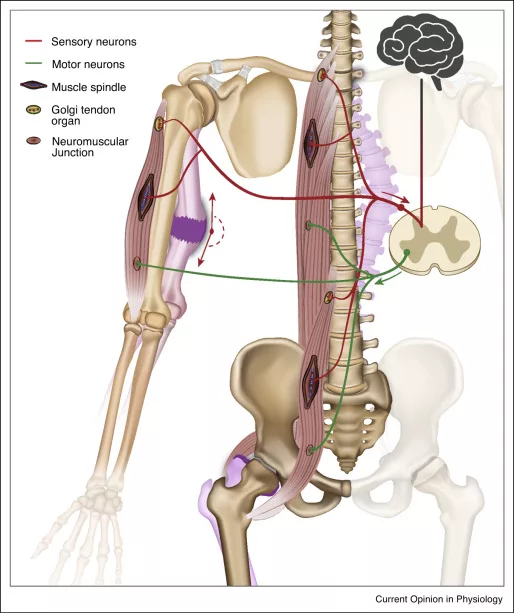
1. Nerve signaling slows
- Peripheral nerves transmit information less efficiently
- Diabetic neuropathy accelerates this
2. Muscle & joint sensors weaken
- Less movement → fewer signals sent to the brain
- Stiff joints provide poorer feedback
3. Brain integration changes
- Stroke or TIA can disrupt sensory processing
- Reaction time increases with age
4. Over-reliance on vision
- When proprioception fades, the brain leans too heavily on eyesight
- That’s why balance worsens at night or with eyes closed
Can Proprioceptive Decline Be Prevented or Reversed?
Yes—very often it can be slowed, stabilized, and partially rebuilt.
The key is intentional challenge, not just exercise.
How to Prevent or Improve Proprioceptive Decline


1. Balance Training (Non-Negotiable)
Simple, daily balance work retrains nerve pathways.
Examples:
- Stand on one foot (hold a chair if needed)
- Heel-to-toe walking along a line
- Weight shifting side-to-side
⏱️ 2–5 minutes, 2–3 times a day beats one long session.
2. Reduce Visual Dependence
Train your body to “feel” position again.
Try:
- Standing with eyes closed for 10–20 seconds
- Light marching in place with eyes closed
- Gentle foot placement drills without looking
⚠️ Always near a wall or counter for safety.
3. Foot & Ankle Re-education (Critical for Diabetics)
Your feet are your main sensory input.
Daily habits:
- Barefoot time on safe indoor surfaces
- Toe spreads and towel scrunches
- Ankle circles and calf raises
4. Slow Strength Training
Strength without awareness doesn’t help balance.
Focus on:
- Slow sit-to-stands
- Controlled step-ups
- Slow lowering (eccentric movement)
This improves signal quality, not just muscle size.
5. Neurological Movement Practices
Some activities are especially powerful:
- Tai Chi – gold standard for balance and fall prevention
- Yoga (chair or standing)
- Feldenkrais or somatic movement
These rebuild the brain-body conversation.
6. Blood Sugar & Circulation Control
For diabetics, this is foundational—not optional.
- Stable glucose protects nerve endings
- Walking improves micro-circulation
- B-vitamin sufficiency (doctor-guided) supports nerves
Warning Signs That Need Attention
If you notice:
- Sudden worsening balance
- Numbness progressing quickly
- Falls without clear cause
➡️ Ask about neurological or physical therapy focused on sensory retraining—not just strength.
A Phoenix72-Style Reframe (Important)
This isn’t “getting old.”
It’s use it or lose it sensory fitness.
Proprioception is trainable at 70, 80, even 90—if you challenge it gently and consistently.
If you’d like, I can:
- Design a 5-minute daily proprioception routine for seniors
- Adapt it specifically for post-stroke or diabetic neuropathy
- Turn this into a Phoenix72 micro-chapter or checklist
Just say the word.
🧠⚠️ Post-stroke visual spatial deficit
Important given how often this is overlooked.
Clues
- Trouble judging distance on one side
- Bumping into door frames
- Hesitation stepping down
This can persist even when strength returns.
🧓 Vestibular dysfunction
Your inner ear helps judge motion and orientation.
Symptoms
- Height feels exaggerated
- Uneven ground feels unsafe
- Worse when turning the head
🧠 Big takeaway
For most seniors, this isn’t one disease—it’s a stacking effect:
aging eyes + slower brain processing + weaker balance feedback
That combo subtly warps distance and height perception.
✅ Practical next steps (high-impact)
- Eye exam (specifically ask about contrast & depth)
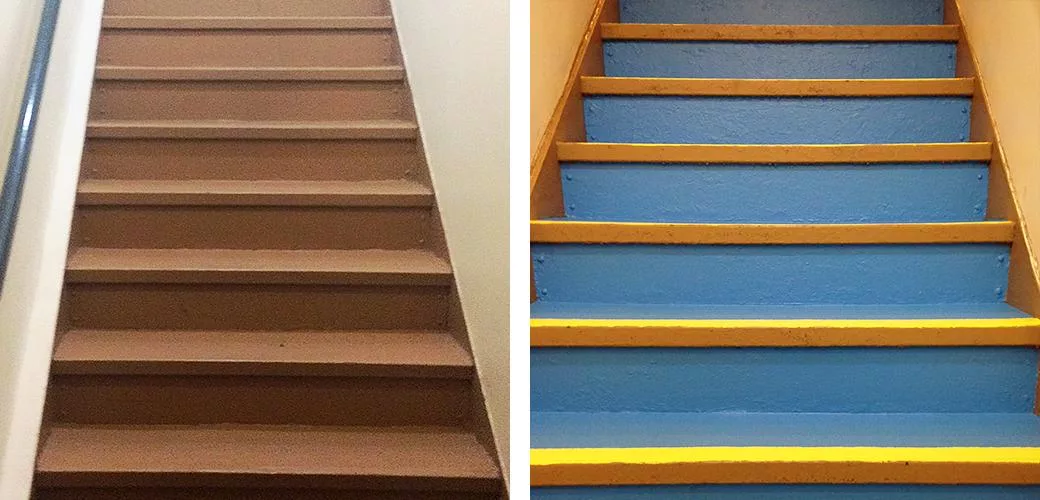
- Good lighting everywhere stairs exist
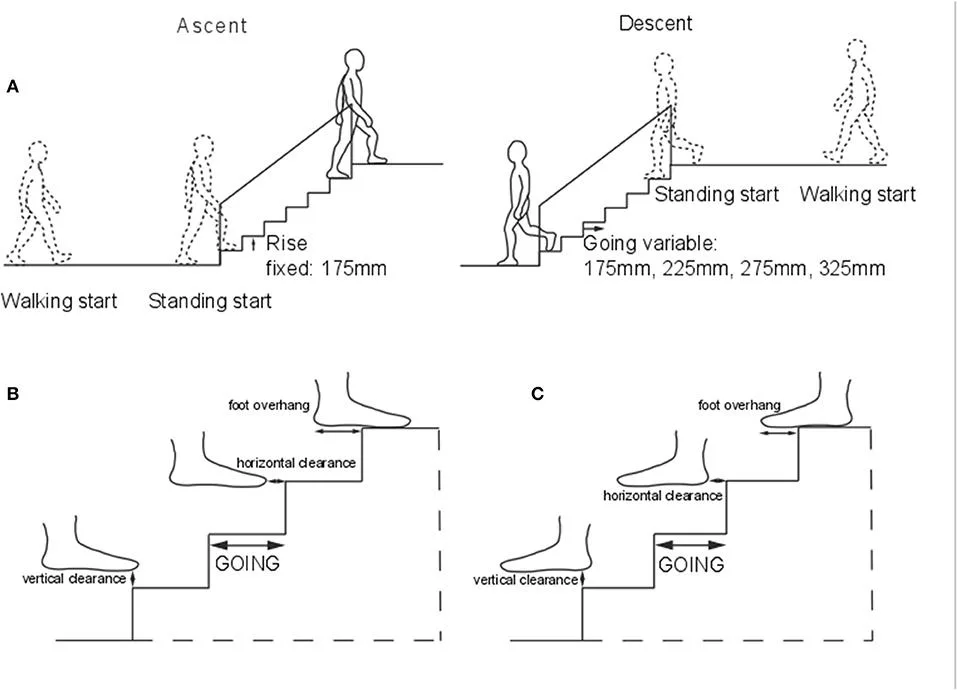
- High-contrast stair edges
- Balance & ankle-strength work (simple daily drills help a lot)
- Avoid rushing—speed magnifies misjudgment
Absolutely. These are simple, senior-safe daily drills that retrain how your eyes, brain, and feet agree on where the ground actually is. Think of them as distance recalibration, not workouts.
Do them slowly, near a counter or wall, once or twice a day. Total time: 8–12 minutes.
1️⃣ The “Edge Finder” Drill (Gold-Standard)
Purpose: Re-teaches accurate step height and drop-off judgment.



How
- Stand facing a single step or curb.
- Slowly lift one foot.
- Tap the edge lightly with your toe (don’t step yet).
- Place the foot fully on the step.
- Step back down the same way.
Reps: 5–8 each foot
Why it works: Your brain relearns the exact location of edges.
👉 Progression:
- Do it once looking straight ahead
- Once looking slightly down
- Once with softer lighting
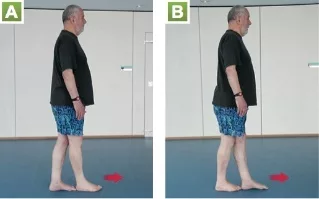
2️⃣ The “Air Step” Drill
Purpose: Improves internal distance prediction before contact.


How
- Stand tall near support.
- Lift one knee as if stepping onto an invisible stair.
- Pause 2 seconds.
- Place foot down gently and accurately.
Reps: 6–10 per side
Key cue: Slow = smarter brain mapping.
3️⃣ Floor Target Drill (Vision → Foot Accuracy)
Purpose: Trains eye-to-foot precision.
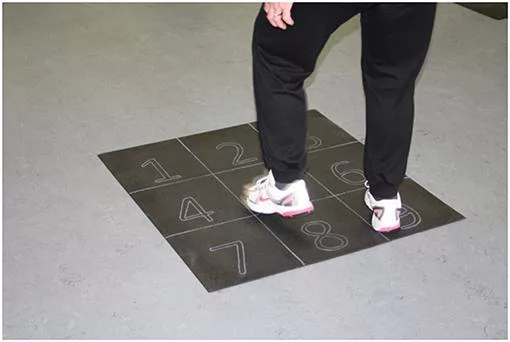

How
- Place a piece of tape or paper on the floor.
- Stand 1–2 feet away.
- Step so your toe lands exactly on the target.
- Reset and repeat.
Reps: 8–10 steps
Upgrade: Change distance slightly each round.
4️⃣ Heel-Hover Drill (Neuropathy-Friendly)
Purpose: Improves depth sensing without impact.


How
- Stand holding a counter.
- Lift one foot.
- Hover heel 1–2 inches above the floor.
- Lower it quietly.
Reps: 8–12 per side
Focus: Silence = accuracy.
5️⃣ Contrast Reset Walk (2 minutes)
Purpose: Fixes depth errors caused by poor contrast.


How
- Walk slowly across different surfaces (tile → rug → wood).
- Look ahead, not down.
- Let your feet adjust automatically.
This retrains the brain’s “auto-pilot” depth system.
6️⃣ One-Foot Pause (Micro-Balance Reboot)
Purpose: Improves real-world stepping confidence.
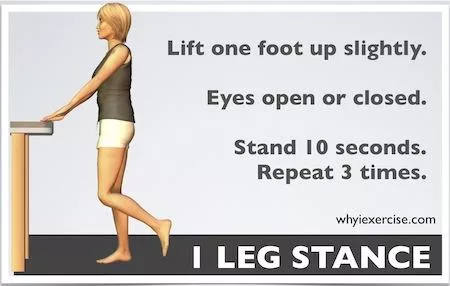
How
- Take a normal step.
- Pause 1–2 seconds on one foot.
- Continue walking.
Do this casually during daily movement.
🧠 Why these drills work
They reconnect three systems at once:
- Vision (where is it?)
- Proprioception (where am I?)
- Motor control (how far do I move?)
That combo is what aging disrupts—and what these drills restore.
⚠️ Safety rules (important)
- Always practice near a wall or counter
- Never rush
- Stop if dizziness appears
- Shoes on, good lighting
🧓 Senior Warrior Tip
Do 2–3 drills daily, not all of them.
Consistency beats intensity—every time.
=====